Common infections are becoming increasingly difficult – and sometimes impossible – to treat.
New data from the World Health Organization (WHO) shows that one in six bacterial infections globally is resistant to standard antibiotics, threatening millions of lives and straining healthcare systems worldwide.
According to WHO’s latest report, antibiotic resistance increased in over 40 percent of the tracked combinations of bacteria and drugs between 2018 and 2023, with average annual increases of 5 to 15 percent.
— Antimicrobial resistance is outpacing advances in modern medicine, threatening the health of families worldwide, says WHO Director-General Tedros Adhanom Ghebreyesus.
The report, based on data from over 100 countries, shows that one in three infections in WHO’s South-East Asia and Eastern Mediterranean regions were resistant to antibiotics, compared to one in five in Africa.
Overuse of antibiotics
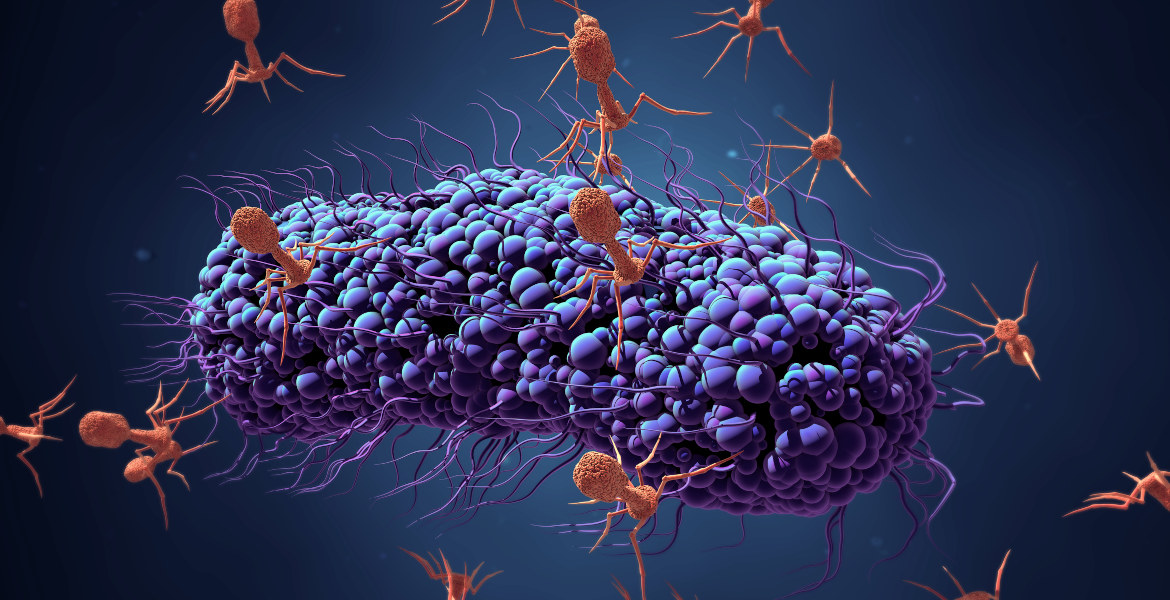
Antimicrobial resistance (AMR) occurs when bacteria, viruses, fungi, and parasites evolve to resist the drugs designed to kill them.
This is primarily driven by overuse and misuse of antibiotics in humans, animals, and agriculture. Poor infection control, limited access to quality medicines, and inadequate sanitation and clean water further exacerbate the problem.
WHO estimates that bacterial AMR directly caused 1.27 million deaths in 2019 and contributed to nearly five million deaths globally. Without action, experts warn that resistant infections could cause an estimated €2.7 trillion in global GDP losses annually by 2030.
“We must innovate”
The greatest danger comes from certain disease-causing gram-negative bacteria, as their protective outer shell makes them difficult to kill and they often develop drug resistance. E. coli and K. pneumoniae, two common causes of bloodstream infections, show alarming resistance levels.
Globally, more than 40 percent of E. coli strains and 55 percent of K. pneumoniae strains were resistant to third-generation cephalosporins – the first-line treatment for many serious infections. In parts of Africa, levels exceed 70 percent.
— Our future also depends on strengthening systems to prevent, diagnose and treat infections and on innovating with next-generation antibiotics and rapid point-of-care molecular tests, declares the WHO Director-General, who as usual calls for more resources to be allocated to vaccination programs.
— We must use antibiotics responsibly, and make sure everyone has access to the right medicines, quality-assured diagnostics, and vaccines, the statement reads.